Focused ultrasound from outside the body can safely and reversibly open the blood–brain barrier in patients with Alzheimer’s disease, researchers in Canada have shown for the first time. The technique could offer a way to bypass the barrier and deliver therapeutic compounds to the brain that can treat Alzheimer’s and other neurologic disorders.
The blood–brain barrier separates the brain’s blood vessels from brain tissue. It regulates what can and can’t enter the brain, protecting it from toxins and pathogens in the blood. But it also presents a problem for the treatment of neurological diseases, because it blocks therapeutic drugs.
“A typical monoclonal antibody is several thousands of times larger than a compound that can readily get across the blood–brain barrier,” explains Nir Lipsman, a neurosurgeon and scientist at Sunnybrook Health Sciences Centre in Toronto. “This size restriction may limit the effectiveness of otherwise useful compounds.”
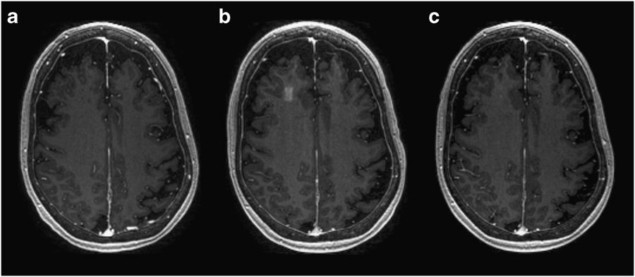
In a phase 1 safety trial, described in Nature Communications, Lipsman and his colleagues first gave five patients with mild-to-moderate Alzheimer’s an intravenous injection of microbubbles, and then focused low-frequency ultrasound on a region in the right frontal lobe of their brains. Real-time imaging in combination with medical dye showed that the blood–brain barrier opened in all patients, and had closed again within 24 hours.
A month later, four of the patients received the treatment again – with the same results. (The fifth patient developed a respiratory illness between the two procedures, which the researchers say was unrelated to the study.) None of patients showed any signs of brain haemorrhaging or swelling, or cogitative decline, on the days of the procedures or during follow-up examinations.
The ultrasound is delivered by a helmet-like device consisting of 1024 transducers, with a frequency of 220 kHz, and is guided by an MRI scan to the target area of the brain. The ultrasound causes the microbubbles to vibrate and rapidly increase and decrease in size, which physically separates the cells of the blood–brain barrier.
“The blood–brain barrier is a complex structure comprised of, among other things, a thin layer of cells held together by tight junctions,” explains Lipsman. “Opening the blood–brain barrier with ultrasound is a physical pulling apart of those tight junctions, and creating space between the cells provides compounds circulating in the blood with better access to the brain across the blood–brain barrier.”
While focused ultrasound could be used to enable the delivery of potentially therapeutic drugs to the brain, Lipsman says there is also pre-clinical evidence that opening the blood–brain barrier without therapeutic compounds present can reduce peptides and proteins that play a role in Alzheimer’s disease.
“Our study is the first demonstration of non-invasive, focal blood–brain barrier opening in humans, for any indication,” Lipsman told Physics World. “It is a necessary first step to designing future studies of opening the blood–brain barrier in patients, where the goal is either using focused ultrasound alone or together with a potential therapeutic for a wide range of brain conditions.”
In the autumn, the team at Sunnybrook plan to start a phase 2 trial that will investigate the safety and efficacy of the technique in a larger group of patients with Alzheimer’s.
Researchers at Sunnybrook are also currently conducting a clinical trial to test whether focused ultrasound can improve the delivery of chemotherapy to brain tumours. Lipsman told Physics World that to date they have treated five patients.
Nathan McDannold, research director of the Focused Ultrasound Laboratory at Brigham and Women’s Hospital in Boston – who wasn’t involved in the study, but has worked extensively with some of the team in the past and helped develop the technology – told Physics World that this trial is a “critical step forward in moving this technology to patients, as it shows that it can be achieved safely and repeatedly”.
“In the field of Alzheimer’s Disease, numerous promising drugs have been developed that have failed in clinical trials,” McDannold says. “Could these drugs be effective if we can enhance their delivery across the blood–brain barrier?”
According to McDannold, similar questions exist for delivering drugs to treat Parkinson’s Disease and brain tumours, and for neuroprotection after stroke or traumatic brain injury. “As more studies like this one emerge showing that this can be achieved safely in patients, I expect that we will see many studies testing therapeutics that are not effectively delivered to the brain,” he says.