Hypofractionated and ultrahypofractionated radiation therapy – increasing dose per fraction to enable significantly fewer overall treatments – promises to unlock significant wins for public and private healthcare providers as well as the radiation oncology teams at the patient end of cancer treatment. While the drivers for hypofractionated procedures such as stereotactic body radiotherapy (SBRT) have been clear for some time – improved patient experience, increased patient throughput and reduced cost of care – the challenge now is to identify new treatment tools and protocols to realize these clinical and economic outcomes at scale.
For starters, clinicians need the ability to maintain submillimetre accuracy and precision throughout treatment delivery – identifying the target location in the body; automatically detecting, tracking and correcting for target motion; and accurately repointing the beam in real-time to support the clinical use of smaller margins to reduce the side-effects of treatment. Between treatment fractions, radiation oncology teams also need tools to efficiently and seamlessly rework treatment plans to account for anatomical changes (see “Adaptive planning”, below). What’s more, none of this cutting-edge functionality can come at the expense of system versatility or patient throughput.
Put another way: the new standard in hypofractionated radiation therapy will be a treatment system that can deliver the highest level of accuracy and precision to both stationary and moving targets, along with the “workhorse versatility” to efficiently treat the full range of clinical indications.
Workhorse versatility
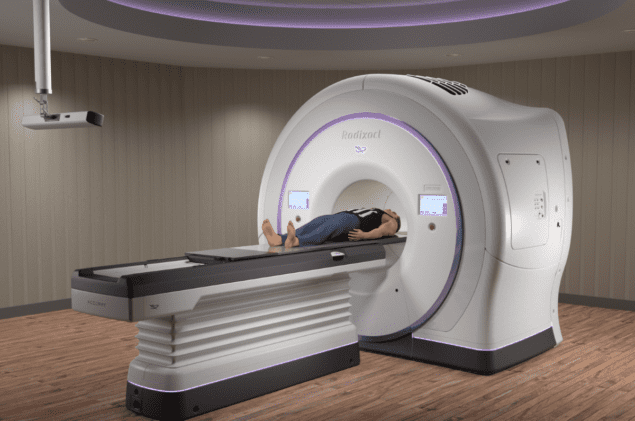
A case in point is Accuray’s Radixact Treatment Delivery System, a helical radiotherapy platform that employs a continuously rotating gantry and unique dynamic collimation system to enable highly conformal dose delivery to diverse tumour sites throughout the body. Radixact has now been upgraded to incorporate motion-tracking and correction algorithms (collectively known as Synchrony) from Accuray’s flagship CyberKnife Treatment Delivery System, a robotic radiotherapy platform widely deployed in treating a range of disease indications using stereotactic radiosurgery (SRS) and SBRT.
We’re not waiting for the target to move and then going there – we’re going to where the target will be proactively.
Andrea Cox, Accuray
This enhanced capability means that the Radixact System with Synchrony is now able to track and synchronize the delivery beam to the target position as the tumour moves. In effect, dose is delivered continuously to the moving tumour target – with the accuracy and precision required for hypofractionated radiotherapy (i.e. tight margins and steep dose gradients) as well as for standard radiotherapy procedures.
“We are the only vendor able to detect targets during treatment, track that motion whether it is regular or irregular, and correct for it in real-time during treatment delivery, with no need for inefficient pausing or gating,” notes Andrew DeLaO, senior director, marketing, at Accuray. “What’s more, target detection and tracking is possible using either fiducial markers or without fiducials, using the patient’s anatomy.”
For targets that move unpredictably – as a result of digestion or bladder-filling, for example – intrafraction imaging detects the motion so that the Radixact System with Synchrony can synchronize the treatment beam to the detected target position as it moves. For targets that move cyclically – as a result of the patient’s breathing – the system anticipates the target’s position using predictive motion-modelling algorithms and continuously synchronizes to that position in real-time based on images captured during each treatment session.
Software aside, it’s Radixact’s unique collimation system (comprising ultrafast multileaf collimators and dynamic jaws) that enables real-time motion correction of the treatment beam. “We’re not waiting for the target to move and then going there – we’re going to where the target will be proactively,” explains Andrea Cox, senior director, product strategy, at Accuray.
She continues: “What we’ve learned over the years [with CyberKnife] is that a patient’s breathing pattern changes from moment to moment as well as day to day – i.e. their breathing actually changes as they relax during the few minutes that it takes to deliver a course of treatment. To take account of this, the model created prior to treatment is always updated in real-time with new images acquired during treatment delivery.”
Ahead of the curve
Just last month, Accuray unveiled the first clinical customer for the Radixact System with Synchrony – the Froedtert and Medical College of Wisconsin Clinical Cancer Center at Froedtert Hospital in Milwaukee, Wisconsin. Folded into that announcement was news that the Froedtert and MCW radiation oncology team has already treated the first patient – a 45-year-old man with lung cancer – using the new-look system, with Synchrony tracking the lung tumour in real-time as it moved with the patient’s breathing while automatically adjusting the treatment beam to keep it targeted on the tumour.
“In our hospital network we’ve seen an increase in the use of hypofractionation – for example, SBRT – as part of the cancer treatment, making it critically important that we are able to safely deliver the correct amount of dose precisely to the tumour, even to those that move such as tumours in the thorax, abdomen and pelvis,” explains X Allen Li, MCW professor and chief of medical physics at Froedtert Hospital.
“With Synchrony we were able to deliver a reduced-margin treatment plan through all three fractions,” he adds. “Total treatment time for a fraction of 18 Gy was 16 minutes door-to-door, similar to our conventional radiotherapy procedures.”
Without motion synchronization, Li and his colleagues point out that a larger treatment field would have been needed to treat the entire path of the tumour movement. Additionally, the treatment time would have been longer as a result of on/off gating of the radiation beam to track the tumour moving in and out of the specified treatment window.
“Our comprehensive pretreatment tests and the initial patient treatment showed us how well the Synchrony technology works in the real-world clinical practice,” Li explains. “As a result, we now have an option for precisely and accurately delivering radiation to tumours as they move, which will expand the range of tumours we can confidently treat and the patients we can help.”
What patients want
For the near term, it’s evident that clinical adoption of hypofractionated radiotherapy is set to accelerate, with a top-down push from healthcare providers towards higher dose per fraction, fewer fractions, compressed treatment times, plus significant workflow efficiencies and lower cost of care.
In parallel, says Cox, there’s growing demand from patients for the benefits associated with hypofractionated treatment schedules – in essence, fewer clinical visits and a faster return to family and friends. “If you imagine a patient with a choice of going in for 30 conventional treatments over a six-week period or going in for five hypofractionated treatments in a one-week period – and for the same clinical outcome – there have to be some pretty compelling reasons for them not to choose the latter.”
- Accuray will be exhibiting at booth 3405 during the ASTRO Annual Meeting in Chicago, IL, from 15-17 September. For more information, download the Accuray ebook: Hypofractionation in the Age of Value-Based Care.
Adaptive planning
Patients are complex systems in every sense. Between treatment sessions, they gain and lose weight; their stomach, bladder and bowel contents change; their organs may shift, rotate or deform; and their tumours may shrink, move or rotate.
The holy grail of online adaptive radiotherapy (ART) is not so far away
Andrew DeLaO, Accuray
Trouble is, traditional radiotherapy regimes rely on a single snapshot of the patient at the start of treatment, with most clinics limited in their ability to reimage patients and bound by rigid-body matching that does not account for any geometric deformations in patient anatomy. A plan attuned to the initial simulation can therefore become suboptimal as treatment progresses, rendering it unusable for hypofractionated or ultrahypofractionated radiotherapy.
“The holy grail is online adaptive radiotherapy (ART) and what we’ve done with the Radixact System with Synchrony is to take significant steps in that direction – a level of automation that allows the user to ‘set and forget’ to some degree,” says Andrew DeLaO, senior director, marketing, at Accuray.
He adds: “After every treatment, the Radixact System with Synchrony actually takes the dose that was delivered, deconstructs that dose and puts it back on the daily image so that you can see what that dose looks like versus the original plan. Offline planning tools automatically identify cases for review and possible plan adaptation using a red-yellow-green flag scheme.”
Equally significant is the use of automatic recontouring to accelerate plan adaptation, while maintaining the integrity of the original treatment plan versus tumour coverage, dose limits for organs-at-risk and overall toxicity.
“The online ART future is not so far away,” says DeLaO. “Where we’re heading is radiation oncology teams able to dynamically change the treatment plan in real-time during a treatment session while the patient is on the table.”




