Developed specifically for verification of stereotactic treatment plans, IBA Dosimetry’s latest innovation in patient quality assurance (QA) combines film-class measurement resolution with the workflow efficiency of a digital detector array
The myQA SRS detector will eliminate patient QA bottlenecks associated with high-precision stereotactic radiosurgery (SRS) and stereotactic body radiotherapy (SBRT) treatments, allowing medical physicists to compare dose distributions – measured versus calculated – in minutes rather than hours and significantly enhancing patient throughput in the process. That’s the claim of IBA Dosimetry, a German supplier of specialist QA products and services to radiation oncology clinics, ahead of the official unveiling of myQA SRS at the virtual ASTRO 2020 Annual Meeting this week.
For context, SRS has generated significant traction – and clinical success – in the treatment of single and metastatic tumours in the brain. By exploiting multiple narrow beams from different directions, SRS is able to deliver conformal, high-dose radiation in one or a few fractions while minimizing collateral damage to surrounding healthy tissue and organs at risk. Similar progress is evident in the stereotactic treatment of tumours elsewhere in the body – for example, in the lungs, liver and spine, where these techniques are referred to collectively as SBRT.
Notwithstanding the growing clinical adoption of stereotactic treatment systems, the extreme physics of SRS/SBRT – focusing high-dose radiation very precisely on a small lesion and having it fall off as quickly as possible – represents a non-trivial dosimetric and QA challenge for the medical physics team. Put simply: it’s not easy to confirm targeting accuracy and dose-distribution accuracy when the stereotactic treatment volume can be as small as a few millimetres in diameter – and doubly so when the existing QA options for SRS/SBRT are unsatisfactory, claims Sandra Kos, product manager for patient QA solutions at IBA Dosimetry.
“While film provides excellent precision in terms of dose resolution,” she explains, “it is cumbersome to use, time-consuming and temperamental, owing to the uncertainties in handling, calibration and development. On the other hand, 2D diode arrays and ion-chamber arrays are able to generate results rapidly, but lack the necessary spatial resolution and error-detection sensitivity for SRS/SBRT QA.” With myQA SRS, Kos argues, that accuracy versus efficiency trade-off no longer applies. “We have created a unique SRS/SBRT QA solution that delivers film-class resolution along with the proven workflow efficiency of a digital detector.”
QA reimagined
If that’s the back-story, what of the device-level innovation? The core sensor in myQA SRS exploits a silicon complementary metal-oxide-semiconductor (CMOS) technology platform, which enables a compact design, fast read-out and high pixel density along the x and y coordinates (with each pixel representing a radiation-sensitive element comprising a photodiode, capacitor and three transistors). All of which yields a significantly enhanced digital detector for stereotactic patient QA.
In the clinic, that patient QA process demands a spatial resolution comparable to film (approximately 0.4 mm) in order to detect and analyse errors in SRS/SBRT treatment plans. While ion chambers, for example, have a proven QA track-record supporting standard radiotherapy techniques – including intensity-modulated radiation therapy (IMRT) and volumetric modulated arc therapy (VMAT) – they lack the resolution needed to deal with the extreme dose gradients characteristic of SRS/SBRT beam delivery.
Typical SRS QA detector arrays seen in clinical use today offer a pitch (distance between measurement points) of 2.5 mm or larger and have limited field sizes. In SRS/SBRT, that granularity is insufficient and necessitates dose interpolation to fill in the “dead points” between pixels – estimates that, in turn, can lead to dose-peak errors. “With the myQA SRS we can decrease the pitch by a factor of 10 [versus standard arrays] and multiply the total number of channels by a factor of 100,” explains Arianna Giuliacci, a nuclear engineer who heads up the testing programme for myQA SRS within IBA Dosimetry. As such, the myQA SRS provides a spatial resolution of 0.4 mm, with more than 100,000 pixels across a large active area of 12×14 cm2.
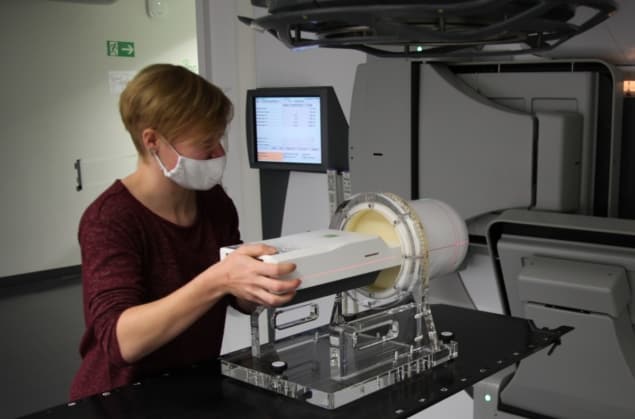
Right now, Giuliacci and her colleagues in Schwarzenbruck, Germany, are focused on physical characterization of the myQA SRS detector versus key performance metrics like thermal stability, measurement precision, reliability and robustness. Using IBA’s in-house clinical set-up, the team has also evaluated dosimetric response of the detector at clinical photon fields and compared performance to ionizing chambers – including measurements of small-field beam output factors and percentage depth-dose curves. “In parallel,” Giuliacci adds, “we have integrated the detector in a treatment planning system, with subsequent irradiation of clinical plans and gamma analysis yielding high pass rates.”
QA best practice
With the in-house testing programme well advanced and third-party clinical evaluation to follow by year-end, myQA SRS is being lined up for full commercial release in the second quarter of next year. Even now, though, the potential upsides for clinical end-users are evident. For starters, the active area of the device (at 12×14 cm2) promises significant time savings in the QA of patients with several treatment volumes, helping medical physicists to confirm that planned SRS treatments are delivered accurately versus the complex dose distributions required for single-isocentre, simultaneous irradiation of multiple lesions.
“There is no need for the physicist to prepare multiple plans or choose which targets they want to QA, as everything can fit in one QA plan and one irradiation session,” explains Kos. “The size of the detector clearly helps to verify mono-isocentric plans with multiple targets.”
Ease of use and reliability also underpin the custom development of a cylindrical SRS/SBRT phantom that’s compatible with static and rotational treatment delivery. As a result, the combined detector–phantom assembly removes uncertainties in set-up, calibration and QA checks, notes Kos, while the QA plans can be verified and cross-checked independently in the same phantom using the myQA SRS detector, different ionization chambers and film. At the same time, the detector’s wireless Gantry Sensor+ provides accurate measurement of linac rotation angles to support rotational treatment plans.
For Kos, the enhanced capabilities of myQA SRS are part of the bigger picture in which independent QA plays a pivotal role in the validation of SRS/SBRT treatments. “Independence is a fundamental requirement for successful QA,” she concludes. “We can check patient QA outcomes without being influenced by possible malfunctions in the radiotherapy equipment chain, and we can ensure peace of mind and confidence that our customers are doing QA in the right way.”
As such, myQA SRS is compatible with all commercial SRS/SBRT treatment systems, including C arm, O-shaped or robotic linacs in a range of clinical set-ups.
Small-field innovation
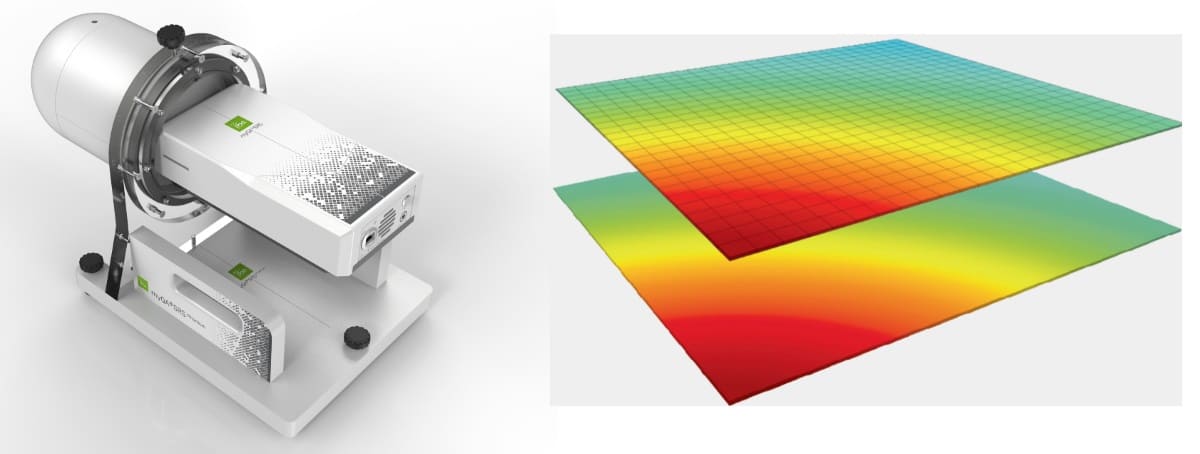
SRS/SBRT target volumes can be as small as few mm diameter and are treated with field sizes of 1×1 cm2 or less. The myQA SRS detector (shown left, with phantom) uses silicon CMOS technology to measure the dose distribution of such a 1×1 cm2 field with 625 measurement points (illustrated in the visualization, right). The schematic shows there is no need for interpolation between measurement points, ensuring unprecedented accuracy for the high dose gradients typical of SRS/SBRT treatment plans. In addition, the myQA SRS offers more than 100 measurement points for a 5 mm stereotactic cone plan.



