Theragnostic radiotherapy involves the use of large amounts of functional imaging data to create a personalized radiation treatment plan tailored to both the geometric and biological attributes of a patient’s tumour. Speaking at the recent AAPM Annual Meeting, Eric Paulson from Froedtert and Medical College of Wisconsin discussed the development of this new treatment approach.
“Theragnostic radiotherapy is an emerging technique, still in its infancy,” Paulson told the conference delegates. “The hypothesis is that non-invasive biological images can be used to derive optimized, non-uniform prescription doses that can then be used in treatment planning.”
Conventional radiotherapy relies on accurate tumour delineation, combined with optimal alignment of the radiation beam to the target, to achieve successful treatments. But radiotherapy can still fail – due to high tumour burden, tumour proliferation or tumour hypoxia, for example. It has been shown, however, that controlled dose escalation can overcome radiation resistance for several tumour types. It may also be possible to lower doses to radiosensitive tumours, thus reducing overall toxicity. In both cases, theragnostics could play a significant role.
One potential approach, which is already employed in some clinics, is to create a “biological target volume”, using PET to identify regions of hypoxia or high tumour burden. But there are challenges with using PET, Paulson explained, including low spatial resolution and high costs. Instead, he proposes the use of a panel of multiparametric quantitative MR imaging (qMRI) techniques to measure parameters such as cell density, oedema, oxygenation, vascular permeability and blood flow.
Hardware options
While this imaging panel could be performed using a standard MRI scanner, the introduction of MRI-guided radiotherapy systems such as ViewRay’s MRIdian Linac or Elekta’s Unity could permit repeat imaging during a course of therapy. This opens up the possibility of adaptive therapy based on functional, rather than just morphological, changes.
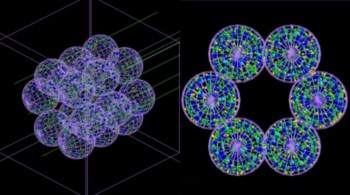
Different scanners, however, may employ different field strengths, RF coils, pulse sequences and so on. So does the hardware used affect the qMRI parameters? Paulson and colleagues examined the performance of three scanners at their Institution: 3T and 1.5T MR simulators and a 1.5T MR-linac.
The team used a Eurospin TO5 phantom to test the T1 and T2 bias of the three scanners. For T1 bias, the 3T simulator, 1.5T simulator and MRI-linac exhibited accuracies of 11.4%, 13.8% and 10.3%, respectively, with consistent overestimation of T1 values across the three systems. The respective accuracies for T2 bias were 4.5%, 6.8% and 11.7%, in this case with consistent underestimation. In all systems, the repeatability was very good, at between 0.1 and 1.1%.
The researchers also examined apparent diffusion coefficient (ADC) bias using a diffusion weighted imaging (DWI) phantom. They saw good agreement between the three scanners, with an accuracy of between 2.0 and 2.6%, and a reproducibility of 1.4%.
Paulson also demonstrated the feasibility of acquiring qMRI in vivo, sharing examples of glioma and rectal adenocarcinoma images. He noted that each panel of images was acquired in less than 15 minutes. The next step, therefore, is to determine how to use these images to create personalized dose prescriptions.
Exploiting the data
The panel of MRI techniques produces a set of parameters, each reflecting a different biological aspect of disease. These could be used individually, or combined using regression models or machine learning. “The question now is which parameter to select. This requires prospective evaluation for each tumour site,” said Paulson.
Other decisions to be made include which dose prescription function to utilize, and whether to create the treatment plan using dose painting by contours (in which a threshold defines low- and high-risk regions) or dose painting by numbers (where each tumour voxel is assigned a specific dose based on phenotype). “This is all still very much in the research realm,” Paulson pointed out.
And once this process has been defined, can biologically-based treatment plans be created using existing planning systems? Paulson demonstrated that the Elekta Monaco planning system can create a dose painting by numbers plan without requiring any modifications.
The final step is treatment delivery. For non-uniform dose distributions that deliver escalated doses to high-risk sub-regions, management of intrafraction motion is of the utmost importance. One potential option is to use an MR-guided radiotherapy system to perform retrospective dose reconstruction and accumulation. Looking further ahead, the blue-sky target is real-time adaptive radiotherapy, in which the treatment plan is continuously adapted with each new anatomy update from the MRI.
“Theragnostic radiotherapy has great potential to further personalize radiation therapy,” Paulson concluded. “However, significant progress in a number of areas is still required before large multi-centre clinical trials using theragnostic radiotherapy can begin.”