Electron beams offer dosimetric advantages for treating superficial targets while sparing underlying organs-at-risk (OARs). Standard electron treatments, however, are still performed using generic or patient-specific cut-outs placed in the electron applicator. Replacing these cumbersome cut-outs with a multileaf collimator (MLC) would profoundly improve clinical workflow and enable advanced delivery techniques.
Previous studies have shown that electron collimation using a photon MLC (pMLC) can achieve similar quality plans to cut-out collimation, for treatments with a reduced source-to-surface distance (SSD) of 60–70 cm. The increased in-air scatter of electrons makes a short-as-possible SSD dosimetrically preferable. However, it could also lead to collisions for certain beam directions, making support of SSDs greater than 70 cm essential. With this aim, researchers in Switzerland have investigated the use of a pMLC for electron treatments with SSDs of up to 100 cm (Phys. Med. Biol. 63 025017).
“For standard electron treatments, the main benefit of switching to a pMLC is the improved clinical workflow, because patient-specific collimation would no longer require fabrication of cut-outs and won’t need to attach an accessory to deliver electron beams,” explained Silvan Mueller from Inselspital and the University of Bern. “On a bigger scope, it would lay the foundations for the implementation of advanced techniques such as modulated electron radiotherapy (MERT) or mixed beam radiotherapy (MBRT).”
Calculation accuracy
To predict dose distributions of pMLC shaped electron beams, the researchers used a multiple source Monte Carlo beam model, ebm70, and a Monte Carlo dose calculation. The ebm70 beam model was originally commissioned at an SSD of 70 cm and designed for electron beams shaped with a Millennium 120 pMLC. Here, the team investigated its use with SSDs of up to 100 cm, and three treatment units: a Clinac 23iX and a TrueBeam equipped with a Millennium 120 pMLC, plus a Novalis Tx with a high-definition MLC.

They found no substantial differences in dose calculation accuracy among the three treatment units. Comparing ebm70 with the commercial dose calculation eMC, used clinically for cut-out collimated electrons, revealed similar accuracy between the two. Measurements in a water tank generally agreed with ebm70 dose calculations to within 3% or 2 mm.
Clinical considerations
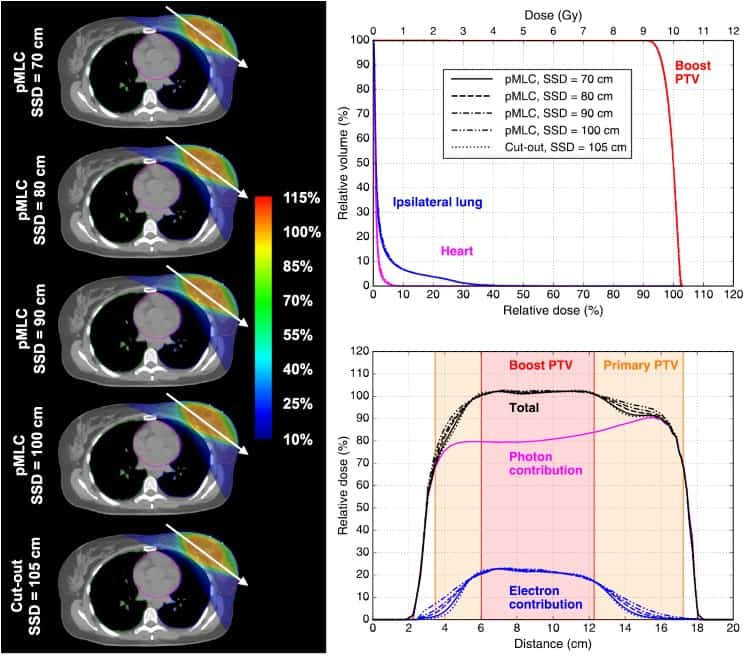
The researchers next considered a series of clinical cases. For each case, they created a cut-out plan with typical clinical settings, plus a deliverable pMLC plan with a similar planning target volume (PTV) dose homogeneity. They examined two breast boost cases, using SSDs of 70–100 cm.
For a left breast boost using a single electron field (1E) at 18 MeV, pMLC plans failed to achieve a homogeneity index (HI) within 3% of the cut-out plan, though dose coverage of the boost PTV was similar for all plans. At SSDs of up to 90 cm, pMLC plans delivered similar mean doses to the ipsilateral lung and the heart as the cut-out, increasing slightly at 100 cm (by up to 0.3 Gy). The volume of normal tissue exposed to the low-dose bath (V10%) was similar for the two plans at an SSD of 70 cm, increasing for the pMLC plan as SSD increased.
For a right breast boost, with a 6 MeV 1E field, the pMLC plan only achieved an HI within 3% of the cut-out plan at an SSD of 70 cm. The mean dose to the ipsilateral lung was slightly increased (by up to 0.3 Gy) for all pMLC plans compared with cut-out plans. V10% of normal tissue was also higher for the pMLC plans, by up to 299% at an SSD of 100 cm.
For the breast boosts, the researchers also created MBRT plans using one electron field and two tangential 3D conformal photon fields (1E2X). The 1E2X plans for the left breast boost (using 12 MeV electrons) exhibited similar dose homogeneity, dose to OARs and V10% of normal tissue for all pMLC and cut-out plans.
“For most of the cases, we believe that MBRT is superior to electron-only treatments,” said Mueller. “The reason for this is the fundamentally different characteristics of photon and electron beams, which allows advantages of one particle type to compensate for disadvantages of the other.”
The team also created pMLC plans for sternum and testis (1E) and parotid gland (1E2X) treatments, with SSDs of 75, 80 and 80 cm. For these three cases, pMLC plans yielded similar or only slightly degraded values for HI and mean dose to OARs, compared with the cut-out plans.
The authors conclude that for each case, a pMLC treatment plan with similar quality to a cut-out plan could be found. They note that for cases with OARs located close to the target in the lateral direction (such as the sternum case), or for 6 MeV electron beams used at an extended SSD, OAR doses were slightly increased.
Mueller and colleagues are now working on dynamic mixed beam radiotherapy. “This advanced MBRT technique combines photon dynamic trajectories with modulated electron beams,” he explained. “Thus, even more degrees-of-freedom are accessed with dynamic couch and collimator rotation. We believe this technique could bring plan quality for targets with at least some superficial part to the next level, using only hardware available on conventional treatment units.”



