Hypofractionated radiotherapy – in which higher doses of radiation are delivered over fewer treatment sessions – offers advantages for both patients and healthcare providers. Completing their treatment in fewer weeks means that patients require less trips to the hospital, less time off work, and reduced transportation and parking costs. For the hospitals, faster patient throughput can increase treatment capacity and reduce costs.
An increasing body of research demonstrates that hypofractionation is effective and feasible in many tumour types. And at this week’s ASTRO Annual Meeting, new results from two clinical studies reinforce the viability of this treatment technique.
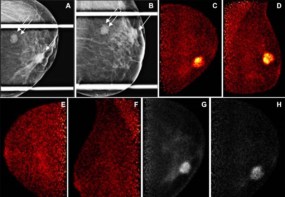
Faster breast-cancer treatment
Speaking at an ASTRO plenary session, principal investigator Frank Vicini reported the results of NRG/RTOG 1005, a phase III trial performed at 276 sites across the USA, Canada, Switzerland, Israel, Hong Kong, Japan, Republic of Korea and Singapore. The study found that for patients with high-risk, early-stage breast cancer, a three-week course of radiotherapy with a concurrent boost is equally safe and effective as four to six weeks of treatment.
For patients with a low risk of recurrence, previous studies have shown that hypofractionated radiotherapy can be used to reduce treatment times following breast-conserving surgery. Patients with higher risk disease require an additional radiation boost to the lumpectomy site, which has been demonstrated to reduce the risk of local tumour recurrence by 20–30%. But if this boost is delivered after the radiotherapy, it adds at least another week to the treatment duration, negating the benefits of the hypofractionation.
“Our objectives were to determine if local recurrence for a boost delivered concurrently with hypofractionated whole-breast irradiation over three weeks was no worse than local recurrence for a boost delivered sequentially,” explained Vicini, a radiation oncologist at GenesisCare, noting that the study exclusively examined patients with high risk for local recurrence.
The trial randomized 2262 patients to receive either conventional or hypofractionated whole-breast irradiation (WBI). The conventional treatment comprised WBI delivered over four to five weeks (50 Gy in 25 or 42.7 Gy in 16 fractions), followed by a sequential boost (12 or 14 Gy) to the tumour bed delivered over six to seven days. Patients in the second group received hypofractionated WBI over three weeks (40 Gy in 15 fractions), with the boost (8 Gy in 15 fractions) delivered concurrently. Most patients (81%) were treated using 3D conformal radiotherapy, the remainder received intensity-modulated radiotherapy.
At a median follow-up of 7.4 years, the three-week treatment was found to be non-inferior to the longer treatment for local recurrence. The five-year and seven-year rates of in-breast tumour recurrence were 1.9% and 2.6% in the hypofractionated group, compared with 2.0% and 2.2% in the conventional group.
“Just as critical, the treatment-related adverse effects were similar,” said Vicini. “There were no statistically significant differences in the distribution of any of the adverse effects, with overall toxicity very low.” He noted that at three years, there were also no differences in cosmetic results between the two treatment groups.
“This approach cuts treatment time for these patients in half,” Vicini noted. “Now the comfort level is there to say to higher-risk patients, ‘I can offer you this option, and it works just as well’.”
Next, the researchers plan to investigate whether more patients, such as those whose cancer has spread to the lymph nodes, can benefit from this three-week approach. They will also examine whether it’s possible to shorten the overall treatment time even further.
Treating high-risk prostate cancer
Also highlighted at the ASTRO conference, a phase III trial performed at 12 sites in Canada demonstrated that men with high-risk prostate cancer can be treated with just five weeks of radiotherapy.
“If we treat high-risk prostate cancer patients conventionally it’s about eight weeks of radiation therapy, the idea was to decrease the number of days that the patients come to the hospital,” explained lead author Tamim Niazi, from McGill University and Jewish General Hospital.
While previous studies have confirmed the safety and efficacy of moderately hypofractionated radiotherapy for patients with low-, intermediate- or mixed-risk prostate cancer, the Prostate Cancer Study 5 (PCS5) is the first randomized trial in to show the same results specifically in men with high-risk disease.
The trial randomized 329 patients with high-risk prostate cancer to receive either conventionally fractionated prostate radiation (76 Gy in 38 daily sessions) or moderately hypofractionated radiation (68 Gy in 25 daily sessions). All patients also received radiation to the pelvic lymph nodes and long-term androgen deprivation therapy.
“At seven years from randomization, the overall survival for these high-risk prostate cancer patients is about 82%, almost identical between the two arms,” said Niazi. “Prostate cancer-specific survival was 95 to 96.4% at seven years, again almost identical. Importantly, distant metastases-free survival at seven years is almost identical, almost 92% in both arms.”
The team noted that side effects were also similar between the treatment arms, with no grade 4 toxicities in either, and no significant differences in grade 3 or higher acute and delayed genitourinary and gastrointestinal toxicities.

A glimpse into the future of radiation therapy
“This is the first moderate hypofractionated radiation therapy exclusively in high-risk prostate cancer patients,” Niazi concluded. “The survival outcomes were pretty much identical, therefore we conclude that hypofractionated radiotherapy is as effective as conventional fractionation, with similar and acceptable toxicity. Moderate hypofractionation radiotherapy should be considered as a new standard-of-care for external-beam radiotherapy of high-risk prostate cancer patients.”
Looking further ahead, Niazi says that one future path could be ultra-hypofractionation – reducing the number of fractions further to potentially just five treatments for suitable patients.