The Society of Nuclear Medicine and Molecular Imaging (SNMMI) Annual Meeting took place this week in Anaheim, CA. Here are some selected research highlights from this year’s conference.
Interim scan helps guide prostate cancer therapy
Researchers at Technical University Munich have shown that adding an interim scan during prostate cancer therapy can help guide treatment. They found that PSMA (prostate-specific membrane antigen) PET imaging of patients with metastatic castration-resistant prostate cancer (mCRPC) after two cycles of 177Lu-PSMA radioligand therapy has a significant predictive value for patient survival.

In phase 2 trials, 177Lu-PSMA therapy has shown promise for treating mCRPC patients. The therapy typically involves a preliminary PSMA PET scan to identify eligible patients. But while interim PET scans have shown high predictive value for lymphoma patients, this concept has not yet been explored in prostate cancer patients undergoing 177Lu-PSMA therapy.
The retrospective analysis, conducted at Klinikum rechts der Isar, included patients who underwent 68Ga-PSMA11 PET/CT at baseline and after two cycles of 177Lu-PSMA therapy. The researchers used in-house developed software, qPSMA, to evaluate the whole-body tumour burden.
“Tumour response was assessed by the changes in PSMA-avid tumour volume from baseline to the second PSMA PET using three classification methods,” explains first author Andrei Gafita. “We found that tumour response assessed on interim PSMA PET after two radioligand therapy cycles was associated with overall survival. While further analyses involving clinical parameters are warranted, this analysis paves the way for use of interim PSMA PET in a prospective setting during 177Lu-PSMA radioligand therapy.”
Early biomarker reveals degenerative neurologic disease
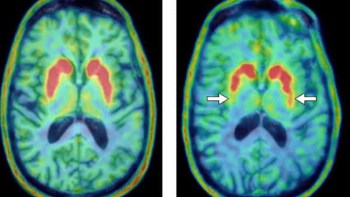
A multicentre study has revealed how a novel radioligand can differentiate progressive supranuclear palsy (PSP) from similar brain disorders. PSP can be difficult to diagnose as its symptoms are often similar to those of Parkinson’s disease and dementia. These latest findings enable earlier and more reliable diagnosis of this rare brain disorder.
“Currently, PSP can only be definitively diagnosed post-mortem by examining region-specific tau deposits in the brain,” explains Matthias Brendel from LMU Munich. “Future interventional trials targeting tau in PSP would strongly benefit from biomarkers to validate the specific presence of the tau deposits and to monitor treatment response during therapy.”

The researchers evaluated patients with suspected tau pathology in clinically diagnosed PSP. They performed PET using the radioligand 18F-PI-2620 on 17 patients with probable or possible PSP, along with 10 healthy controls and seven disease control patients with multi-system atrophy, Parkinson’s or Alzheimer’s disease.
They observed a significantly elevated mean 18F-PI-2620 standardized uptake value (SUV) ratio in the brain’s globus pallidus and substantia nigra areas in PSP patients compared with the healthy group. In contrast, the disease control group had similar or only slightly elevated SUV ratios when compared with the healthy group.
“My colleagues and I were able to detect an elevated signal in the majority of evaluated PSP patients and could clearly discriminate the PSP group from healthy controls and disease controls,” says Brendel. “Importantly, PSP patients at early disease stages also revealed an elevated PI-2620 signal, which points at the suitability of this ligand as an early PSP biomarker.”
Dosimetry vest personalizes 177Lu-DOTATATE therapy
Researchers at the University of Washington are developing a multi-detector personalized home dosimetry vest that collects data to individualize therapy for patients with neuroendocrine tumours (NETs).

Targeted therapy using 177Lu-DOTATATE greatly increases progression-free survival for patients with metastatic, somatostatin-receptor-2 positive NETs. In the USA, however, patients receive a standardized protocol of four 200 mCi doses, regardless of size or weight. This is safe for the vast majority of patients, but less than optimal for most.
Studies in Europe have shown that tailoring the number of doses based upon toxicity to organs-at-risk (OARs) can more than double survival for such NET patients. Traditionally, this organ dosimetry involves longitudinal imaging sessions over seven days – an expensive approach that is burdensome to the patient. The researchers hope that their wearable monitor will let patients track radiotracer washout at home, enabling personalized 177Lu-DOTATATE therapies in the USA and lowering the cost of treatment personalization worldwide.
“We propose to create a lightweight, low-cost, wearable, patient-specific technology that will allow organ-specific measurements to be made within the comfort of the patient’s home,” explains first author Robert Miyaoka. “The garment will house 15–20 small radiation detectors, strategically placed within the vest based upon the patient’s own anatomy. In addition, the vest will be coupled to a compact electronics pack that will acquire data and send them to a secure website, where medical personnel/software can check the data for quality control in near real-time.”
The patient will wear the vest for a two-minute data acquisition once a day for between seven and 21 days. These measurements, together with a single SPECT/CT image taken 24 hours after 177Lu-DOTATATE administration, will provide dosimetry for all of the patient’s OARs, enabling physicians to tailor the number of treatments based upon personalized dosimetry.
“Preliminary vest results from simulations show that at-home vest measurements made over 7–21 days can provide organ-specific washout rates with precision as good or better than the current accepted gold standard of three to four quantitative SPECT/CT images acquired over seven days,” says Miyaoka.
PET/CT provides earlier diagnosis of tuberculosis
Molecular imaging with 18F-FDG PET/CT can evaluate tuberculosis, identifying diseased areas and providing valuable information to guide therapy. While tuberculosis most frequently involves the lungs, involvement of other tissues and organs – referred to as extra-pulmonary tuberculosis – presents a particular challenge as the disease site is often not accessible for diagnosis.
“In our study, we aimed to evaluate the utility of 18F-FDG PET/CT in the initial diagnosis and response assessment of patients with extra-pulmonary tuberculosis,” explains Bhagwant Mittal from the Postgraduate Institute of Medical Education & Research in India.

Mittal and collaborators examined 93 patients with extra-pulmonary tuberculosis. Patients underwent 18F-FDG PET/CT as a baseline prior to treatment, and then received follow-up imaging after two months and after treatment completion.
The baseline scans detected 176 lesion sites among the 93 participants. In two-month follow-up scans on 47 patients, 21.2% had complete metabolic response (no abnormal lesions), 72.3% had residual disease (persistent lesions, but no new lesions) and 6.4% had disease progression (new lesions). A final scan conducted on 28 patients showed that 28.6% had complete metabolic response, 53.6% showed residual disease and 17.8% had disease progression.
“This study has the potential to change the way we manage tuberculosis patients,” says Mittal. “Our results show that 18F-FDG PET/CT provides a whole-body survey and identifies the disease sites in various organs and tissues in a single study. This helps to provide an early estimation of disease extent, and in suspected cases, helps to identify accessible biopsy sites for obtaining tissue diagnosis. Further, follow-up scans can point towards response to treatment and thus suggest predict a more accurate outcome.”