Surface guidance – in which advanced 3D camera technologies are used to track the patient’s skin surface – is increasingly employed for motion management in radiation treatments. At the recent ESTRO 37 congress in Barcelona, Philipp Freislederer from LMU Munich University Hospital explained the rationale behind surface-guided radiotherapy (SGRT).

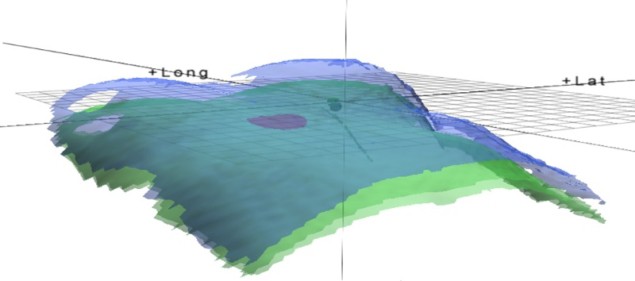
“SGRT uses technology to position and monitor the patient’s external surface to ensure they are in the correct position throughout their radiation treatment,” Freislederer explained. “It matches surface data, in six degrees-of-freedom and in real time, to a reference model captured during planning or at the point of internal imaging in the treatment room.”
SGRT can be applied both for patient setup and during the treatment. Traditionally, daily patient positioning is performed using skin marks to align the patient on the treatment coach, followed by verification with cone-beam CT (CBCT) or MV imaging. Surface guidance offers the advantage of being able to see local deviations in areas without skin marks, increasing the accuracy within such regions of the body.
Freislederer and colleagues performed a study evaluating the setup accuracy of an optical surface scanner (C-RAD’s Catalyst HD) in four treatment regions: head-and-neck, thoracic, abdominal/pelvic and extremities. They analysed 1902 treatment fractions in 110 patients. After positioning the patients using conventional skin marks, 3D deviations were detected by SGRT and using CBCT (as a gold standard).
The team found that SGRT provided similar positioning accuracy to CBCT, without the associated additional radiation exposure. They noted particularly good results in areas with fixed tumour-surface relations, such as the cranium, and lower accuracy when moving from the head to thoracic and abdominal regions.
So could surface guidance replace image guidance? “It’s not clear,” said Freislederer. “Image guidance should still be standard, but maybe for some body regions and some fractions, image guidance could be partially replaced.” He noted that staff training will be essential for accurate positioning, and that the small extra time required for SGRT may impede its acceptance.
Intrafraction monitoring
The other key application of SGRT is intra-fractional monitoring, where surface guidance can constantly monitor the patient position throughout the whole treatment fraction, and any shifts can quickly be observed and accounted for. SGRT can also enable automatic beam holds, an important additional safety feature.
One area where SGRT is particularly useful is to guide deep inspiration breath-hold (DIBH), in which patients hold their breath whilst radiation is delivered. DIBH is employed to limit dose to heart and lungs, particularly during radiotherapy to the left breast, and the beam is switched on and off as the patient breathes.
Freislederer described a prospective study at LMU Munich examining the use of SGRT for DIBH in 168 patients with left-sided breast cancer. The study confirmed the benefits of DIBH. Dose to the heart was reduced compared with free breathing and, in about 25% of patients, the heart was seen to move completely out of the radiation field. He noted that it is possible to perform DIBH using skin marks, but that surface guidance delivers additional safety features and removes the need for invasive procedures such as spirometry.
Another important use of SGRT is in whole-brain radiotherapy using open masks, for patients who cannot tolerate fixed full masks. Instead, a chin immobilization mask can be used and SGRT employed to monitor any residual movements throughout the treatment. Tolerance settings can be employed to perform automated beam hold if required.
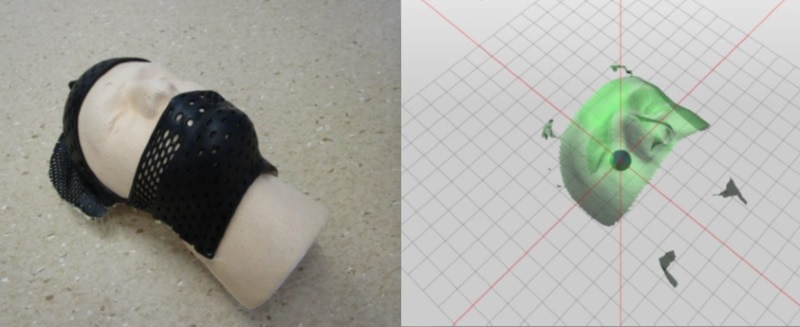
One step further, there’s the possibility of using SGRT to monitor the patient’s position during frameless cranial stereotactic radiosurgery (SRS). Here again, the patient wears a mask with an opening for their eyes and nose and is monitored continuously (about twice per second) during beam-on. Using a mask material with a high contrast to skin enables auto-cropping of the open region in the recorded images.
This approach demonstrated an accuracy of better than 1 mm for isocentric couch rotations. The reproducibility was better than 0.15 mm/0.05° for small translations and better than 0.25 mm/0.1° for small angular deviations – in the same range as for frame-based SRS.
Finally, surface guidance can be applied for respiratory-correlated 4DCT scanning. Here, SGRT could serve as an ideal surrogate with which to measure the patient’s breathing, without the need for belts or other sensors. One important consideration is the best place to measure motion. Freislederer suggested that this could be the upper abdomen on the right side of the patient.
Limitations and possibilities
While there are many applications for SGRT in radiotherapy, Freislederer cautioned that there are limitations too. Surface guidance is not suitable for gating or tracking in stereotactic body radiotherapy of the lung or liver, for example. Respiration is not stable and a breathing curve prediction algorithm would be required. Also, there are currently no models available that accurately correlate motion of the patient’s surface and tumour.
Freislederer concluded that surface guidance offers great potential for fast and accurate patient positioning and continuous intra-fractional motion surveillance during radiotherapy. He emphasized that staff training is essential and that vendors will need to adapt clinical workflows and standards. “SGRT can provide extra safety, improved accuracy, and the possibilities of implementing new radiotherapy techniques,” he told the delegates. “But one must keep in mind that an extra effort must always be made, such as training, quality assurance and time expenses.”



