Microbeam radiation therapy (MRT) uses synchrotron X-ray beams to deliver spatially fractionated radiation, with extremely high peak doses deposited in the microbeam path and tissue located between the microbeams receiving only a small fraction of this dose. MRT has proved highly effective in treating various tumours in small animals, while selectively sparing normal tissues. However, the mechanisms underlying the therapeutic efficiency of MRT are not well understood.
To shed light on these processes, a research team headed up at the University of Bern has evaluated the anti-tumour efficacy of MRT on a radioresistant melanoma, in comparison with the effects of uniform irradiation (Int. J. Radiat. Oncol. Biol. Phys. 10.1016/j.ijrobp.2019.08.027).

Malignant melanoma is one of the most aggressive cancers and is often radioresistant. “Although the main treatment for melanoma is surgery, in some cases resection is impossible due to the location of the tumour,” explains first author Marine Potez. “We wanted to find an alternative treatment for these tumours.”
With this aim, Potez and colleagues implanted radioresistant melanoma cells into the ears of mice. Roughly 10 days later, they divided the mice into three groups: 47 to be treated with MRT; 28 treated with conventional broad beam irradiation; and 26 non-irradiated controls. They performed all experiments using synchrotron X-rays produced at the European Synchrotron Radiation Facility.
The researchers treated the conventional group using a homogeneous 7.5×15 mm beam to deliver 6.2 Gy to the tumour. For the MRT treatments, the 7.5×15 mm irradiation field was covered by 37 quasi-parallel, 50-μm wide microbeams, with a peak dose of 407.6 Gy and a valley dose of 6.2 Gy.
Measuring tumour size before irradiation, on the day of treatment and then daily showed that both types of radiotherapy impeded melanoma growth compared with controls. Tumour volume doubled in 2.1 days in the control group, 3.7 days in the conventional group and 6 days in the MRT group. MRT significantly attenuated growth, with tumours shrinking from days 4 to 8 and then slowly growing again. Conventional irradiation, however, could not stop progression even temporarily, with tumours in this group exhibiting almost exponential growth throughout the study.

Underlying mechanisms
To investigate why MRT offers better tumour control than conventional radiotherapy, the researchers first examined the impact of radiation on tumour blood vessels. They found that MRT altered blood vessel integrity and significantly reduced blood perfusion into irradiated tumours. At day 5 after irradiation, for example, 68.5% of vessels in the MRT group were perfused, compared with 86.3% and 81.5% for conventional and control groups, respectively.
Irradiated tumours also exhibited a reduced tumour cell proliferation index compared with controls, from day 2 in the MRT group and day 5 in the conventional group. MRT resulted in lower proliferation rates, with maximum divergence on day 9 when the proliferation indices were 14.5% and 70.9%, for MRT and conventionally treated tumours, respectively.
Immunostaining excised tumour slices for senescence – in which cells no longer divide but are still metabolically active – revealed a marked increase in senescence after MRT from days 2 to 9, compared with the other groups of mice.
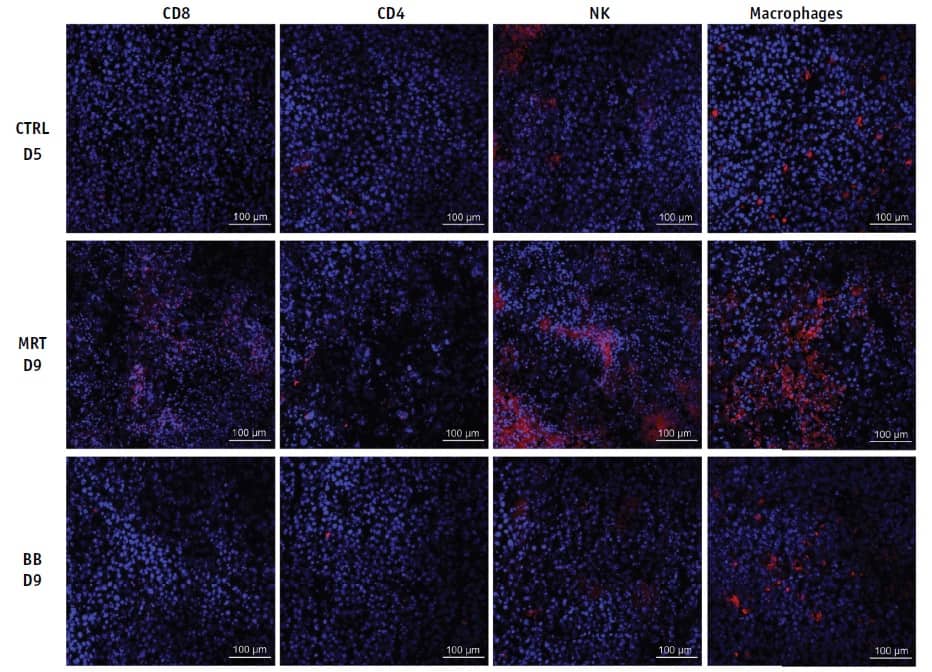
This MRT-induced senescence significantly enhances the production of chemokines involved in recruitment of monocytes (a white blood cell involved in immune processes) in tumour tissue, which the team confirmed using Bio-Plex immunoassays. This led to a massive influx of immune cells (macrophages, natural killer cells, CD4+ and CD8+ T lymphocytes) in MRT-treated tumours from day 5 to day 12, which can induce inflammatory and anti-tumour immune responses.
“We observed that the first tumour response after MRT was vascular damages and senescence,” says Potez. “We hypothesized that the high influx of immune cells, recruited by the senescence-associated secretory factors, caused the vasculature impairments.”
The researchers suggest that MRT represents a promising candidate for new clinical trials to explore the clinical relevance of these anti-tumour effects. Currently, however, MRT is in the pre-clinical stage, including trials on pets with spontaneous tumours and on pigs, which provide a good intermediary between small lab animals and human patients.

Phase-contrast CT reveals impact of microbeam radiotherapy
Potez notes that due to the particular irradiation geometry of MRT, positioning and treatment planning are still under development for patients. “Also, MRT can only be performed at third-generation synchrotrons to fulfil the requested parameters, such as the dose rate and parallel-non divergent microbeams,” she says. “To be more accessible for patients, the development of compact sources is ongoing.”
In the next stage of this project, the researchers are characterizing the infiltrating immune cells. “We are also testing different treatment protocols with multiple irradiations and ports, and we are combining MRT with nanoparticle injection,” Potez tells Physics World.



