Photodynamic therapy (PDT) kills cancer cells using a photosensitizing drug that localizes within tumours. When irradiated with a specific wavelength of light, the drug produces reactive oxygen species that kill nearby cells.
In recent years, metronomic PDT, which uses long-term (hours to tens of hours) and low-dose photoirradiation, has shown promise in treating cancers within internal organs. Metronomic PDT can employ miniaturized optical devices to emit light anywhere in the body. To ensure continuous, localized light delivery, however, this approach, requires stable fixation of such devices to internal tissue surfaces.
Surgical suturing — the standard choice for device fixation — is unsuitable for use with fragile tissues or organs, or those that change shape or move. If the light source shifts even slightly away from the tumour, the drug will not be activated and the antitumour effect will not occur. To address this challenge, scientists from Japan have developed a bioadhesive light-emitting device for minimally-invasive metronomic PDT of cancers in delicate organs (Nature Biomed. Eng. 10.1038/s41551-018-0261-7).
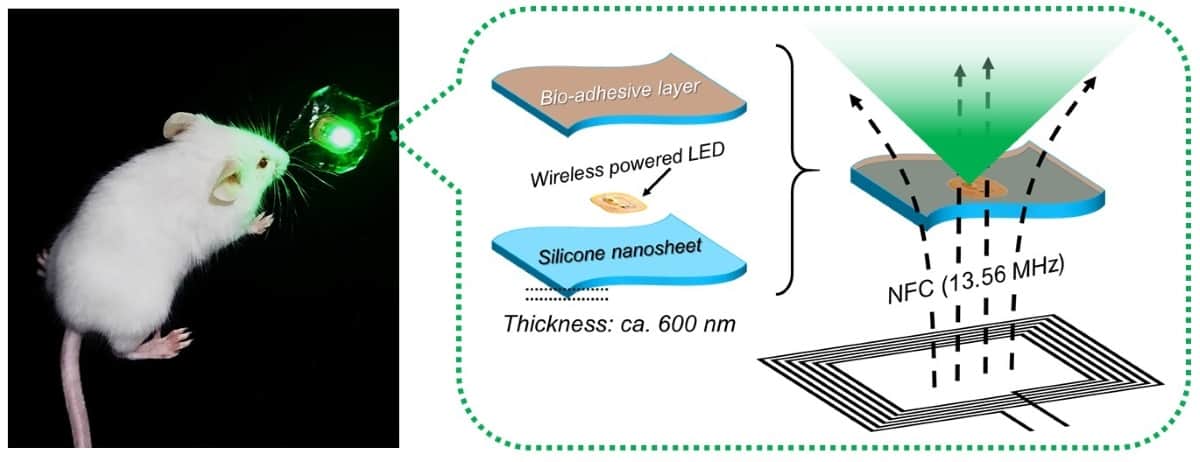
The team created an implantable optoelectronic device that can be stably fixed onto the inner surface of animal tissue using elastic poly(dimethylsiloxane) nanosheets. The nanosheets were modified with the mussel protein-inspired bioadhesive polydopamine, which can stabilize the device onto wet tissue for more than two weeks without suturing or medical glue. The device contains light-emitting diode chips that are wirelessly powered by near-field-communication technology, enabling continuous light delivery to the tumour.
To test its effectiveness, the researchers subcutaneously implanted the devices into tumour-bearing mice and injected them with the photosensitizing agent photofrin. They then exposed the animals to red and green light (with peak emission at 630 and 530 nm, respectively) at approximately 1000-fold lower intensity (below 100 μW/cm2) than used for conventional PDT, for 10 consecutive days.
The experiment showed that tumour growth was significantly reduced overall. In addition, the tumour was completely eradicated, in six of 10 tumours irradiated with green light and one of 10 irradiated with red light. The researchers note that the temperature increase of the device (for both red and green light) was less than 1 °C even after 24 h of continuous operation, conferring negligible risk of thermal tissue damage.
“This device may facilitate treatment for hard-to-detect microtumours and deeply located lesions that are hard to reach with standard phototherapy, without having to worry about the risk of damaging healthy tissues by overheating,” explains Toshinori Fujie from Waseda University. “Furthermore, because the device does not require surgical suturing, it is suitable for treating cancer near major nerves and blood vessels, as well as for organs that are fragile, change their shape or actively move, such as the brain, liver and pancreas.”