Hyperbaric oxygen therapy (HBOT), an established medical treatment that involves breathing pure oxygen in a pressurized environment, could provide a new means to slow the progression, or even prevent the development, of Alzheimer’s disease. That’s the conclusion of a new study from researchers at Tel Aviv University and Shamir Medical Center.
Reporting their findings in Aging, the researchers demonstrate that HBOT can improve cerebral blood flow and cognitive function in mouse models of Alzheimer’s disease, as well as in elderly patients with significant memory loss. They also show for the first time that HBOT can reduce the volume of amyloid plaques in these mouse models. As amyloid plaques are one of the main hallmarks found in the brains of people with Alzheimer’s disease, this gives hope for similar improvements in Alzheimer’s disease patients.
Reduced cerebral blood flow, and the resulting decrease in oxygen supply to the brain (hypoxia) is associated with the onset of dementia and correlates with the degree of cognitive impairment in Alzheimer’s disease. The team hypothesized that developing a technique to target vascular dysfunctions, such as reduced vessel diameters, may offer a way to treat Alzheimer’s disease – a disorder for which there is presently no effective intervention.
Animal investigations
The researchers first examined the impact of HBOT on 5XFAD transgenic mice, which have impaired cognitive abilities. They exposed the mice to HBOT at twice atmospheric pressure for 60 min per day, 20 times over four weeks. Post-mortem staining revealed a significant reduction in amyloid burden in the hippocampus of treated mice, with fewer and smaller plaques than seen in control untreated 5XFAD mice.
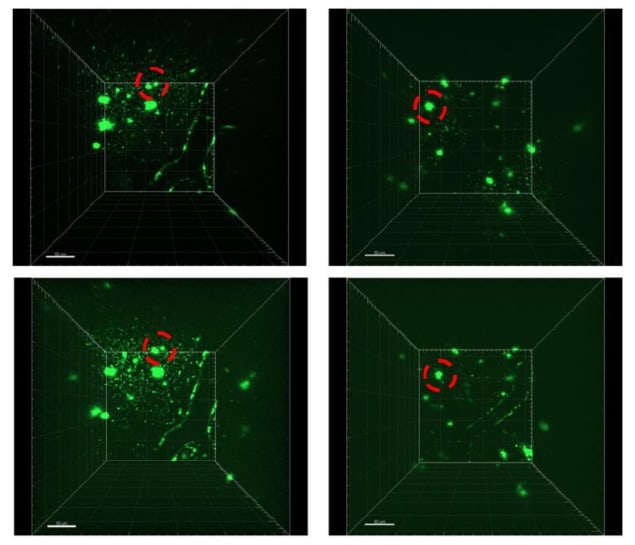
The team also performed two-photon microscopy imaging in live animals to study the dynamics of amyloid plaque formation. Without treatment, pre-existing plaques increased in size over time, with smaller plaques growing the most.
HBOT halted the growth of these small plaques and reduced the volumes of medium-sized and large plaques. Overall, existing plaques in control mice grew by an average of 12.3% over one month, while plaques in treated mice shrank by 40.05% on average.
Using HBOT to increase oxygen delivery to the brain also prevented the formation of new plaques. Over one month, the number of plaques seen in untreated mice almost doubled, while in mice receiving HBOT the number remained constant. Live animal imaging also revealed that HBOT alleviated the reduction in vessel diameter seen in Alzheimer’s disease mice, leading to increased cerebral blood flow and reduced hypoxia.
Finally, the researchers investigated whether these physical responses to HBOT affected the behavioural performance of the mice. They found that HBOT improved the animals’ nest construction abilities and exploratory behaviour, compared with control mice. In addition, control mice showed a decreased spatial recognition and contextual memory performances over time, which was not seen in treated animals.
“We have discovered for the first time that HBOT induces degradation and clearance of pre-existing amyloid plaques – treatment, and stops the appearance of newly formed plaques – prevention,” explains corresponding author Uri Ashery in a press statement.
Clinical study
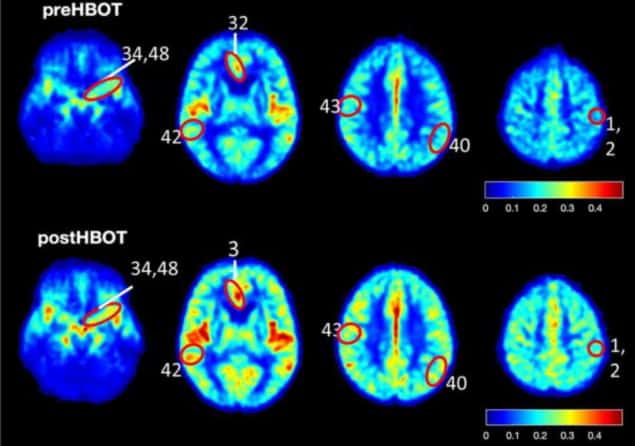
Motivated by these findings, Ashery, co-author Shai Efrati and colleagues treated six elderly patients with significant memory loss with 60 HBOT sessions over three months. Each session included breathing 100% oxygen via a mask at twice atmospheric pressure for 90 min, with 5 min breaks every 20 min. High-resolution MR imaging before and after HBOT revealed that this treatment improved cerebral blood flow in several brain areas, with increases of 16–23%.
The team employed computerized cognitive tests to evaluate the subjects’ cognitive functions before and after HBOT. At baseline, patients attained a mean global cognitive score of 102.4±7.3 (a score of 100 represents the average in their age group), and a lower mean memory score of 86.6±9.2. HBOT improved both measures, increasing the global cognitive score to 109.5±5.8 and the mean memory score to 100.9±7.8.

EEG test could enable early diagnosis of Alzheimer’s disease
“Elderly patients suffering from significant memory loss at baseline revealed an increase in brain blood flow and improvement in cognitive performance, demonstrating the potency of HBOT to reverse core elements responsible for the development of Alzheimer’s disease,” says Efrati.
The researchers conclude that the mouse model findings – combined with the similar effects observed in patients – suggest that HBOT causes structural changes in blood vessels, which serve to increase cerebral blood flow, reduce brain hypoxia and improve cognitive performance. They note that HBOT holds promise for the prevention of Alzheimer’s disease as it not only addresses the symptoms, but targets the core pathology and biology responsible for the advancement of the disease.