
Image guidance plays a vital role in radiation therapy, with on-board kilovoltage cone-beam CT (kV-CBCT) commonly used for patient alignment, motion assessment and adaptive treatment planning. Now, a US–Canadian research team has come up with a brand new application for kV-CBCT: direct visualization of the delivered dose distribution (Int. J. Radiat. Oncol. Biol. Phys. 10.1016/j.ijrobp.2018.12.023).
The team — headed up at Duke University and the University of British Columbia — is investigating the use of an N-isopropylacrylamide (NIPAM) polymer gel dosimeter. Exposure to radiation changes the polymer’s mass density, which manifests as a change in CT image intensity and can be measured by the on-board kV-CBCT.
“The biggest advantage of using an on-board CBCT for dose visualization is that it automatically informs the physicist precisely how the dose is aligned in the same imaging coordinate system used for patient alignment and treatment,” explains first author Justus Adamson from Duke University Medical Center. “Since all modern medical linear accelerators are equipped with CBCT, it can be applied essentially anywhere without need for additional imaging technology.”
The team’s first goal is to use the CBCT polymer gel dosimetry for quality assurance of multifocal stereotactic radiosurgery (SRS) — a treatment that has stringent requirements for spatial accuracy.
Verifying spatial accuracy
In its simplest form, the quality assurance process involves aligning the dosimeter on the radiation delivery system, irradiating it and then acquiring a volumetric image with the on-board CBCT while the dosimeter is still on the treatment device. Finally, the resulting image is processed and used to verify the spatial accuracy of radiation delivery.
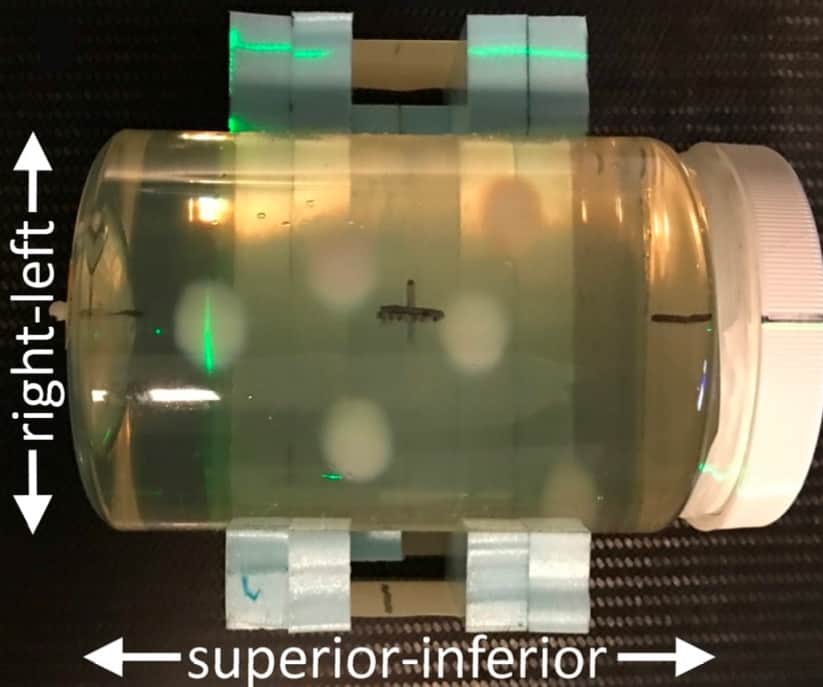
For this study, Adamson and colleagues acquired simulation CTs of a 9.5 cm-diameter NIPAM dosimeter and generated a multifocal SRS treatment plan for delivery on a 6 MV linac with a high-definition multileaf collimator. They designed a 4-arc volumetric-modulated arc therapy (VMAT) plan that delivered 20 Gy to six 1 cm-diameter targets.
Next, the researchers aligned the dosimeter on the treatment table and delivered the plan. They recorded a CBCT scan prior to irradiation and three further CBCT images immediately after. For comparison, they also acquired five diagnostic CTs of the dosimeter 24 hours later.
CBCT images of the irradiated dosimeter clearly showed the delivered dose distribution. The mean contrast-to-noise ratio (CNR) per target was 1.4±0.4 for individual CBCTs and 1.7±0.7 after averaging the three images.
To improve the CNR, the researchers applied a low-pass filter, which increased the CNR to 2.5±1.4. Background subtraction increased the CNR to 2.2±0.3 and 5.8±0.5, with and without the filter, respectively. In comparison, the CNR of single and averaged diagnostic CTs were 5.5±0.4 and 11.6±3.7, respectively.
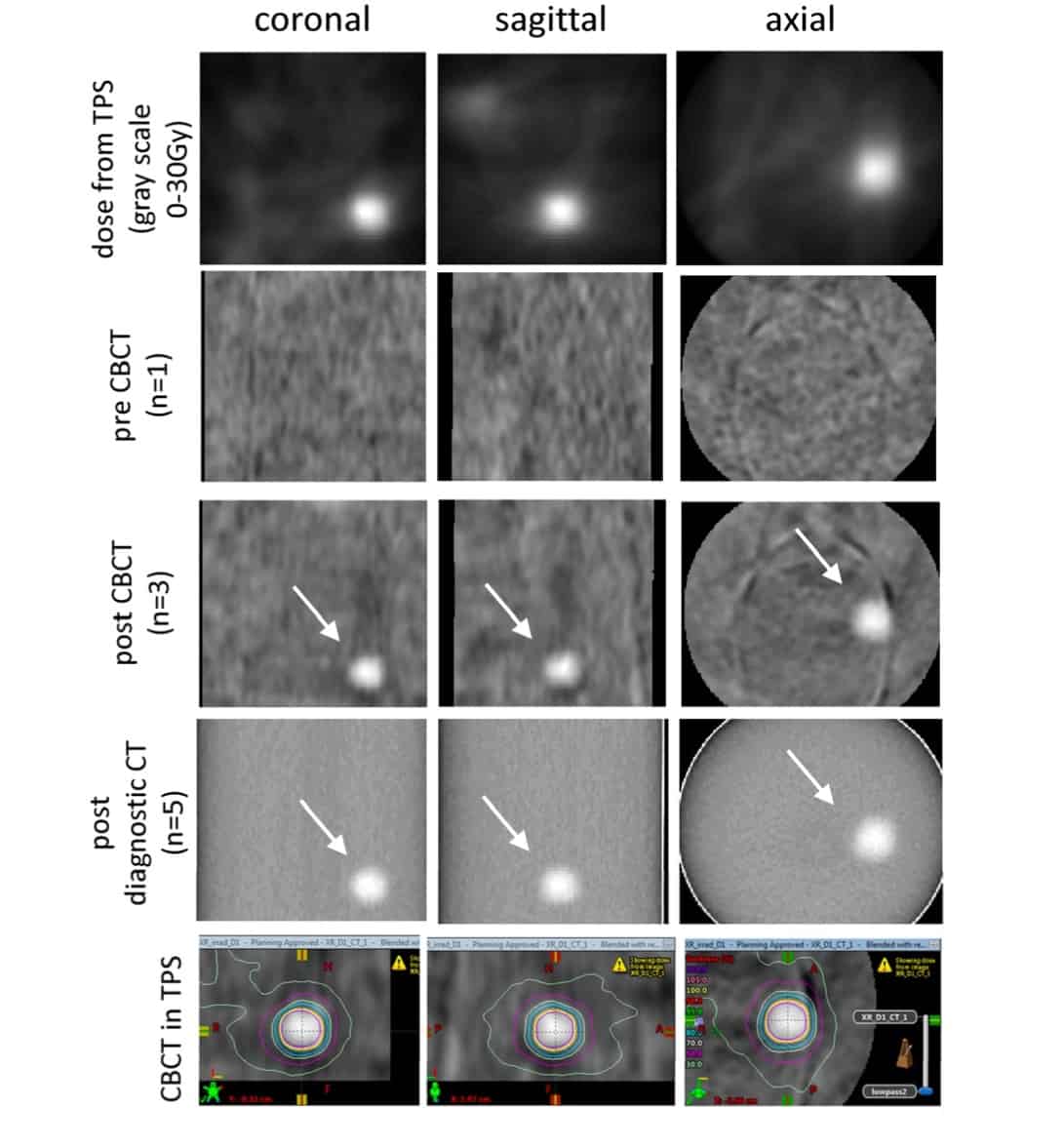
The centroids of prescription isodose volumes from the average CBCT agreed with those from the treatment planning system to within 1.1 mm (range 0.8–1.7 mm). For the diagnostic CTs, the centroids agreed to within 0.7 mm (0.4–0.8 mm).
Absolute dose
Adamson and colleagues also performed an absolute dose comparison using a diagnostic CT of the dosimeter. To do this, they created an absolute dose calibration curve derived from irradiating a second dosimeter with a 3-field plan that included dose gradients.
Profiles of planned and measured dose revealed that the dosimeter yielded a signal that was proportional to dose in the high-dose (above 10–12 Gy) volumes, with 3D gamma pass rates of 94.0% and 99.5%, using 5%/1mm and 3%/2mm criteria, respectively. At lower doses, however, the dosimeter exhibited nonlinear behaviour and poor dose sensitivity.
The researchers concluded that this work demonstrated, for the first time, the potential to visualize a delivered radiotherapy dose immediately after irradiation using on-board CBCT, with sufficient CNR to measure radiation and imaging system coincidence to within 2 mm.
“The accuracy in this proof-of-principle is a good start; however, we’ve already found a number of ways of improving it quite a bit,” says Adamson. “I anticipate that with ongoing improvements we will be able to achieve sufficient spatial accuracy for quality assurance purposes, even for SRS.”
The team is now investigating practical clinical applications where this technology could provide both convenience and value. “One example is radiation isocentre coincidence measurements, or ‘star-shots’,” Adamson explains. “In this case, this technology not only allows for more convenient analysis, using CBCT, but also inherently quantifies coincidence of the radiation and imaging isocentres, which is not possible with a traditional film measurement.”
“We are also actively working on improving sensitivity of the system and better characterizing the dosimeter response in the short timeframe between irradiation and CBCT acquisition,” he tells Physics World.



