
The fundamental advantage of proton therapy lies in its ability to deliver a high radiation dose to a specific depth in the body, known as the Bragg peak, which lies at the maximal penetration depth of the proton beam. After this, the dose rapidly falls off, sparing healthy tissue behind the target.
Conventionally, proton therapy planning relies on estimates of this particle range in the patient, provided by Hounsfield look-up tables (HLUT) that convert CT numbers to stopping-power ratio (SPR). Any uncertainties in these range estimates, however, could result in the actual delivered dose not fully covering the target. To prevent this, proton therapy centres typically add a safety margin of 2.5–3.5% of the proton range plus 1–3 mm, but this can correspond to about 10 mm for deep-seated tumour sites such as the prostate. This safety margin could potentially be reduced using state-of-the-art CT-based methods for range prediction, such as DirectSPR, the direct determination of SPR from dual-energy CT (DECT).
In a study described in the International Journal of Radiation Oncology, Biology, Physics, first author Jonathan Berthold from OncoRay and the Helmholtz-Zentrum Dresden-Rossendorf, together with principal investigator Christian Richter and co-developers, used prompt gamma imaging (PGI) to analyse the accuracy of these range prediction methods. Their study represents the first systematic validation of CT-based proton range prediction in clinical proton beams.
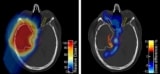
PGI works by detecting the prompt gamma rays produced when the proton beam interacts with atomic nuclei within the patient. The PGI slit camera, developed by IBA, relies on the projection of the emission profile of prompt gamma radiation along the proton path onto a spatially resolved detector through a tungsten knife-edge slit collimator. The resulting one-dimensional prompt gamma distribution, which is obtained for each spot of a pencil-beam scanning treatment, contains information regarding the range of the protons in the patient. For this study, the PGI slit camera was upgraded by mounting it on a floor-based docking system to improve positioning accuracy.
Validation for prostate cancer treatments
The DirectSPR implementation in Dresden, based on a long-term collaboration with Siemens Healthineers, uses CT images at two X-ray energies for direct measurement of a patient’s tissue properties and performs a voxel-wise direct SPR calculation from those DECT scans. The researchers conducted PGI-based validation of proton range prediction using this DECT-based DirectSPR, as well as two other range prediction approaches: a standard HLUT method; and an adapted HLUT optimized by DECT-derived SPR calculation.
They analysed the accuracy of the three approaches using clinical PGI measurements during hypofractionated treatment of five prostate cancer patients (30 fractions in total), with in-room control DECT scans in the treatment position. For each pencil-beam-scanning spot, the team obtained the range shift by comparing the PGI measurement to a control-CT-based PGI simulation. The mean range prediction accuracies were: 0.0 ± 0.5% for DirectSPR; 0.3 ± 0.4% for the adapted HLUT; and 1.8 ± 0.4% for the standard HLUT approach.
“The highest accuracy was reached for the Direct SPR approach, yielding no range deviation for the monitored prostate-cancer treatments,” write the authors. “Our validation confirms the superiority of DECT-derived SPR prediction approaches over current state-of-the-art HULT approach based on single-energy CT.” They hope that this validation of range prediction in patients will support change in clinical treatment planning and foster the clinical implementation of DECT-based planning at other proton therapy centres.
Dual-energy CT for proton therapy planning reaches the clinic
The researchers note that they chose prostate-cancer treatments to evaluate because these contain a highly homogeneous target region, as well as requiring the highest penetration depth in particle therapy. They point out that the comprehensively determined uncertainty of the PGI-based validation was about 1 mm in prostate cancer patients. This is far smaller than the range prediction uncertainty of HLUT-based approaches and DirectSPR used at the Dresden proton therapy facility – an important prerequisite for this first-in-human range validation of the clinically applied technique.
Based on their research, the researchers will extend the application of PGI to other treatment sites, such as head-and-neck cancers. They also plan to use PGI and accompanying CT data acquired within their study to systematically investigate the sensitivity of PGI-based treatment verification to detect anatomical changes during the course of proton therapy.



