Proton therapy is a limited resource that’s available to relatively few cancer patients. But as more cancer centres install single-room proton systems into their radiotherapy clinics, combined proton–photon therapy could provide a practical alternative. The question then becomes: “how can a given number of proton therapy slots be used optimally in a proton–photon treatment?”
In previous studies of combined treatments, intensity-modulated radiotherapy and proton therapy (IMRT and IMPT) plans were optimized separately and then simply combined. Now, a research team headed by Jan Unkelbach from University Hospital Zürich has demonstrated that simultaneous optimization of the two modalities can capitalize better on proton therapy’s ability to reduce normal tissue dose (Radiother. Oncol. 10.1016/j.radonc.2017.12.031).
“In this work, we specifically look at treatment sites where a certain number of fractions is needed to protect dose-limiting normal tissues within or near the target volume,” Unkelbach explained. “These can only be protected through fractionation, and hence both proton and photon fractions should deliver the same dose to these tissues.”
However, parts of the gross tumour volume (GTV) may be eligible for hypofractionation. In this case, most of the dose to the GTV can be delivered with protons. Thereby, healthy tissues away from the target volume benefit from an overall reduction of the photon dose bath.
Case study
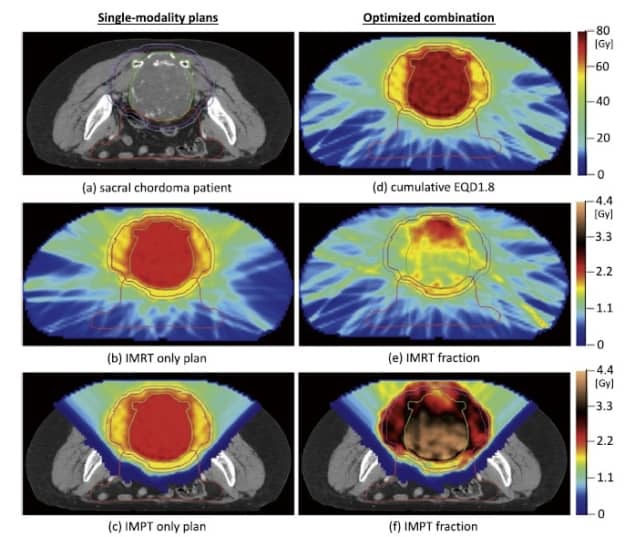
Unkelbach and co-authors demonstrated this concept for a sacral chordoma patient in whom the GTV abuts the rectum, bowel and bladder. Chordomas require high radiation doses to achieve local control, and are treated with simple proton–photon combinations at some institutions (such as MGH in Boston). For this patient, most of the GTV could be hypofractionated with protons, however, protecting the rectum, bowel and bladder required fractionation.
To account for fractionation effects, the researchers simultaneously optimized IMPT and IMRT plans based on their cumulative biologically effective dose (BED). While traditional plan optimization evaluates objective and constraint functions for physical dose, in this approach, these same functions are instead evaluated for cumulative BED.
To quantify the benefit of optimized proton–photon treatments, the researchers initially optimized a 30-fraction IMRT plan and a 30-fraction IMPT plan, based on the same set of objectives. They used these single-modality plans to generate a reference plan representing a simple proportional combination, in which the two modalities deliver the same target dose.
The team also created two optimized proton–photon plans: combination 1, which used the same objectives as the single-modality plans; and combination 2, which emphasized integral dose reduction by increasing the weighting for objectives that minimize dose to OARs and remaining healthy tissue.
Dose comparisons
Optimized combination 1, with 10 IMPT and 20 IMRT fractions, generated a conformal treatment plan that delivered the prescribed BED to the target volume. The proton and photon fractions in this plan delivered similar doses to the bowel and rectum overlaying the target, thus protecting these normal tissues through fractionation.
In the GTV, on the other hand, photon fractions delivered a mean dose of 1.7 Gy while proton fractions delivered 3.6 Gy, thereby lowering the integral dose to the gastrointestinal tract compared with the reference plan.
The mean BED4 (assuming an α/β ratio of 4 for healthy tissues) to the bowel was 13.12 Gy for a 30-fraction IMRT plan and 4.85 Gy for the IMPT plan. The reference plan, with 10 proton and 20 IMRT fractions, yielded a BED4 of 10.41 Gy, corresponding (as expected) to approximately one third of the dose reduction possible using protons alone. The optimized combination 1 plan delivered a mean BED4 of 8.63 Gy, corresponding to 54% of the reduction possible with IMPT.
As optimized combination 1 uses the same objective function as the single-modality plans, improvements over the reference plan are distributed over multiple objectives. By shifting most of the benefit to reducing integral dose, optimized combination 2 achieved 78% BED reduction compared with the reference plan, without degrading target coverage or conformity.
Dose-volume histograms showed that the five plans (IMRT, IMPT, reference and optimized combinations 1 and 2) delivered similar target coverage and were similar in the high-dose region of the bowel and rectum, which overlap with the PTV. The main difference was observed in the low-dose region of the bowel, where the optimized combinations improved upon the reference plan.
Finally, the researchers varied the number of proton fractions in a combined 30-fraction treatment from one to 20. The mean BED reduction in the bowel increased with increasing number of proton fractions. With five IMPT fractions, optimized combinations 1 and 2 achieved BED reductions of 36% and 66%, respectively, levels that would require 11 and 20 IMPT fractions in a simple proportional combination of plans.
Clinical options
The authors note that optimized proton–photon therapy could benefit many other clinical indications, such as spinal metastasis with epidural involvement, for example, or large liver tumours abutting the bowel, stomach or duodenum.
“As a next step towards implementation, we will look at the robustness of combined proton–photon treatments with respect to range and setup errors, and apply robust plan optimization techniques to mitigate such uncertainties,” Unkelbach told medicalphysicsweb.



