Myeloma is a blood cancer that develops from plasma cells in the bone marrow and which affects 140,000 new patients each year across the globe. Diagnosis and assessment are usually performed using advanced imaging techniques such as whole-body CT, whole-body MRI (WBMRI) or PET/CT with the radiotracer 18F-FDG. But at present, it is not clear which is the best imaging test to use.
Researchers from King’s College London hypothesized that the greater sensitivity of WBMRI over 18F-FDG PET/CT for detecting myeloma could prove advantageous for patient management. To investigate this further, they compared the diagnostic performance of the two techniques in patients with a suspected or newly confirmed myeloma diagnosis, reporting their findings in the European Journal of Nuclear Medicine and Molecular Imaging.
“Our results showed that imaging with WBMRI changed how patients would have been managed by their doctors in 24% of cases, where review of clinical data alone would have resulted in surveillance only,” explains lead researcher Vicky Goh. “What this ultimately means for patients is improved outcomes from earlier treatment.”
Expert analysis
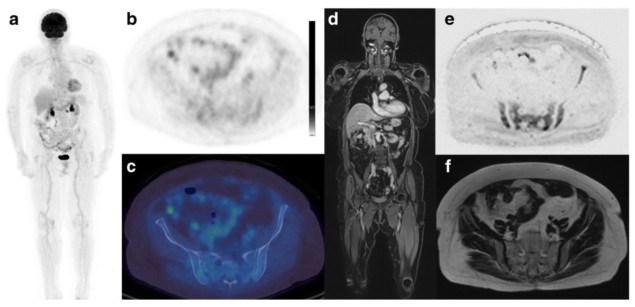
The study included 46 patients who underwent both pre-treatment WBMRI and 18F-FDG PET/CT. Forty-one patients had symptomatic myeloma, three had smouldering (asymptomatic) myeloma and two had multifocal plasmacytoma. The PET/CT and WBMRI scans were reviewed independently by an experienced nuclear medicine physician and radiologist, respectively, who recorded the presence or absence of focal and diffuse disease, as well as the number of focal lesions.
The per-patient sensitivity of WBMRI for detecting myeloma bone disease was 91.3% (42 of 46 patients), compared with 69.6% (32 of 46 patients) for PET/CT and 54.3% for the PET component alone. There were no cases where PET/CT was positive for disease detection and WBMRI was negative.
In 58.7% of patients, WBMRI and the CT component of PET/CT detected the same number of focal bone lesions; in the other cases, WBMRI detected a larger number of such lesions. The researchers note that in 10 patients with negative PET/CT studies, WBMRI detected more than 10 lesions. All three patients with smouldering myeloma had negative PET/CT studies. Two of these patients also had negative WBMRI studies, but the third had focal bone lesions seen on WBMRI and their diagnosis was upgraded to myeloma.
To assess inter-observer agreement, two additional readers (a nuclear medicine physician and radiologist) performed further evaluation in a subset of 12 patients. The readers showed moderate agreement in detecting focal disease using CT and PET. In the WBMRI scans, there was excellent agreement between the two readers in detecting the presence or absence of focal lesions in each patient.
Looking at the impact on clinical management, the researchers found that based on clinical data alone, 32 of the 46 patients would be treated for myeloma rather than undergoing active surveillance. Adding PET/CT to the clinical data resulted in treatment of 40 patients, while adding WBMRI led to 43 of the patients receiving treatment – an additional 7%.
Goh and colleagues concluded that WBMRI detects skeletal disease in a higher number of patients than 18F-FDG PET/CT and also detects a higher number of lesions per patient. Adding the imaging findings to the clinical data led to in a significantly higher proportion of patients recommended for treatment rather than surveillance, although the researchers note that treatment decisions were not statistically different between modalities – either would be appropriate in initial staging.
In a press statement, Goh notes that the study supports national guidance from the National Institute for Health and Care Excellence (NICE) that WBMRI should be performed as a first-line imaging test for suspected myeloma. “Earlier diagnosis and treatment is key to improving patient outcome. Forty percent of NHS hospitals still only perform X-rays, an insensitive test, for diagnosing bone disease in suspected myeloma,” she says. “This clearly needs to change.”
“We offer WBMRI as our first-line test in suspected myeloma patients,” Goh tells Physics World. “Going forward, we are clarifying the role of WBMRI compared to 18F-FDG PET/CT in the treatment setting.”



